Pediatric biliary atresia
When the bile ducts are blocked or when they don't function normally, bile (which is the liquid that carries the waste products) backs up in the liver. This bile backup damages the liver and even endangers the baby's life.
What is pediatric biliary atresia?
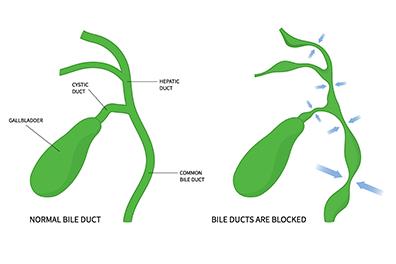
Missing or incomplete bile ducts is a serious condition known as biliary atresia. The bile is normally made by the liver to assist with the digestion of fatty foods. It drains through the small tube of the bile ducts, past the gallbladder and into the intestine.
Blockage of the common bile duct and resulting cholestasis in newborns is surgically managed, and surgery with the Kasai procedure (or Kasai portoenterostomy) can reestablish bile flow in most infants.
Risk factors
Biliary atresia is a rare condition, but the condition is one of the most frequent causes of liver transplantation.
What are the signs and symptoms of pediatric biliary atresia?
Some babies will start to gain weight, then lose weight and have other symptoms such as:
Light-colored stools
Dark-colored urine
Irritability
Yellow discoloration of skin can get worse
How is pediatric biliary atresia diagnosed?
Ultrasound - Performing an abdominal ultrasound may help suggest biliary atresia, but a diagnosis is confirmed by an intraoperative cholangiogram to determine the structures of the bile duct and gallbladder, as well as microscopic evaluation of the liver.
Blood work - Blood work look at the makeup of elements in the blood (bilirubin levels) and specialized scans (cholescintigraphy) further examine the bile ducts and gallbladder.
How is pediatric biliary atresia treated?
The Kasai procedure replaces the infant’s damaged atretic bile ducts with a section of the infant’s intestine. This restores bile flow from the liver to the intestine and prevents liver damage and failure. However, there are times when the scarring has become too advanced and the Kasai operation doesn’t work. For this reason, it’s important to make the diagnosis and perform a Kasai procedure early in the baby’s life.
After surgery, infants must be followed closely for several years for signs of inadequate biliary flow restoration or other complications. We work together with our patients’ families and primary care physicians to coordinate follow-up care.
Pediatric biliary atresia doctors and providers
 Amal Aqul, MDPediatric Hepatologist
Amal Aqul, MDPediatric Hepatologist Sarah Barlow, MDPediatric Gastroenterologist
Sarah Barlow, MDPediatric Gastroenterologist Jorge Bezerra, MDPediatric Hepatologist
Jorge Bezerra, MDPediatric Hepatologist Natasha Corbitt, MDPediatric Surgeon
Natasha Corbitt, MDPediatric Surgeon Diana Diesen, MDPediatric Surgeon
Diana Diesen, MDPediatric Surgeon Barbara Gaines, MDPediatric Surgeon
Barbara Gaines, MDPediatric Surgeon Stephen Megison, MDPediatric Surgeon
Stephen Megison, MDPediatric Surgeon Charina Ramirez, MDPediatric Gastroenterologist
Charina Ramirez, MDPediatric Gastroenterologist Norberto Rodriguez-Baez, MDPediatric Hepatologist
Norberto Rodriguez-Baez, MDPediatric Hepatologist Isabel Rojas Santamaria, MDPediatric Gastroenterologist
Isabel Rojas Santamaria, MDPediatric Gastroenterologist Meghana Sathe, MDPediatric Gastroenterologist
Meghana Sathe, MDPediatric Gastroenterologist